It’s 6am in the morning. I have my arm laid out on a Chux pad on a table in the Pharmacy office with a 20 gauge angiocath sticking out of my AC. The angiocath is held by the shaking hands of a new nurse trying valiantly to stick the needle into my vein. A bead of sweat rolls down her forehead as I say, “You’re doing good. Just keep advancing the needle.”
“I’m not hurting you?” she asks with a worried frown.
“Nope, just fine. Keep going.” I said, distracted by the phone ringing on the desk.
“I think I missed.”
Looking down at my arm and the angiocath, “Yup. Looks like it. Do you want another go at it?”
So why am I subjecting myself to the unskilled ministrations of this nurse? Other than the fact I’m a nice guy and an awesome preceptor and charge nurse? Because her nursing school education failed her.
I’m not saying that her education was sub-par or that she was unable to pass the NCLEX, but that the essential technical skills of a nurse were glossed over. Nursing school is supposed to be a chance to learn. Learn pathophysiology, disease processes, the nursing process and a load of nursing theorists. It should build a theoretical and knowledge based foundation to base one’s practice upon. In addition to knowledge, it is an opportunity to learn the technical skills that one has to call upon as a nurse. Things like inserting Foleys and nasogastric tubes, restraining patients, changing beds (with the patient still in it) and starting IVs. The basic technical skills. I’m not talking about drawing ABGs, performing EKGs, dealing with chest tube drainage systems or interpreting rhythms, skills that are unit specific and taught in relation to that unit, but basic/slightly advanced nursing skills.
As we were about to begin, the nurse confided in me, “I’ve never started an IV.”
“Never? Like never at all?” I ask incredulously. “Not in school, not in your preceptorship?”
“No. We weren’t allowed.”
“Why on earth? (actually thinking WTF) not?”
“They said it was something we would learn on the job.”
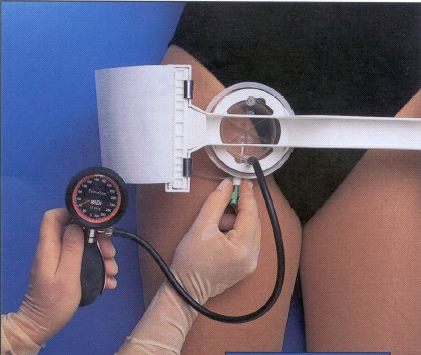
That’s delusional thinking on the part of the faculty. Like many other hospitals, ours has an IV team, a dedicated crew of nurses whose sole duty is to place IVs, whether peripheral, midlines or PICCs. During the day this isn’t a problem, but after 2300, we’re pretty much S.O.L. (shit out of luck). Sure we still have an IV nurse, but 9 out of 10 they’re busy placing a PICC or at another facility across town. A new peripheral site does not top high on their priority list. It comes down to the floor nurse to step up and place a line themselves. Frequently though, the patients we get the “practice” on in the middle of the night are not the best subjects, hence why I was on the table.
There are not enough educational opportunities to teach our multitude of new nurses the skill, no, art of inserting an IV. Hell, there’s not enough opportunity for the rest of us to keep our skills sharp (no pun intended…). I was a lucky one. I did my preceptorship in a relatively busy ER, where I had multiple opportunities to poke needles into folks in varying states of consciousness and I got adept, not great, but able to start lines. However, that skill is pretty much rusty and as out of shape as I am due to a lack of practice. How then are we supposed to provide that opportunity to newer grads?
It seems a large disservice by that school to deny the opportunity for their students to learn such a vital and practical skill. I agree, it’s not always the best thing to have legions of eager students roaming the halls to stick unsuspecting patients with large bore angiocaths. It’s a great way to deter frequent flyers return if they were greeted with such a sight, but alas it isn’t going to happen. But what happened to starting it on each other? That’s how we learned. I won’t soon forget having my classmate John digging around my hand with an 18g trying to poke my elusive dehydrated vein. That didn’t feel good. But it was how we learned.
So why the vitriol Wanderer you may ask? It’s because we recently hired 9 nurses to the the night shift, most of whom are new grads, most without the previous experience of starting IVs. Some never dropped an NG, placed a Foley, given charcoal or done a large time-consuming dressing change. It leaves gaps in the team that places a larger impetus on the experienced nurses on the unit to step up and fill the holes while trying to figure out how to get these folks up to technical speed. And when not everyone is willing to step outside their norm, it makes it a little more stressful.
“So, OK, figure out what you did wrong?” I ask as she arranges a new set on the table.
“No. No clue. Any suggestions, words of wisdom?”
“One thing, go in steeper than you did. My veins are a little deeper, so go in steep, when you get the flash, go just a little further then flatten it out.” I replied demonstrating what I meant.
“OK, you ready?”
“As I’ll ever be.” Wish I could say it was a successful ending, but I would be lying. We work together soon, so I’ve resigned myself to be a pin cushion. If it helps, well, then it’s worth it. Just wish her nursing school would had delivered so I wouldn’t need to be that pin cushion.